ROLE OF IMMUNO-THERAPY IN TREATMENT OF LYMPHOMA
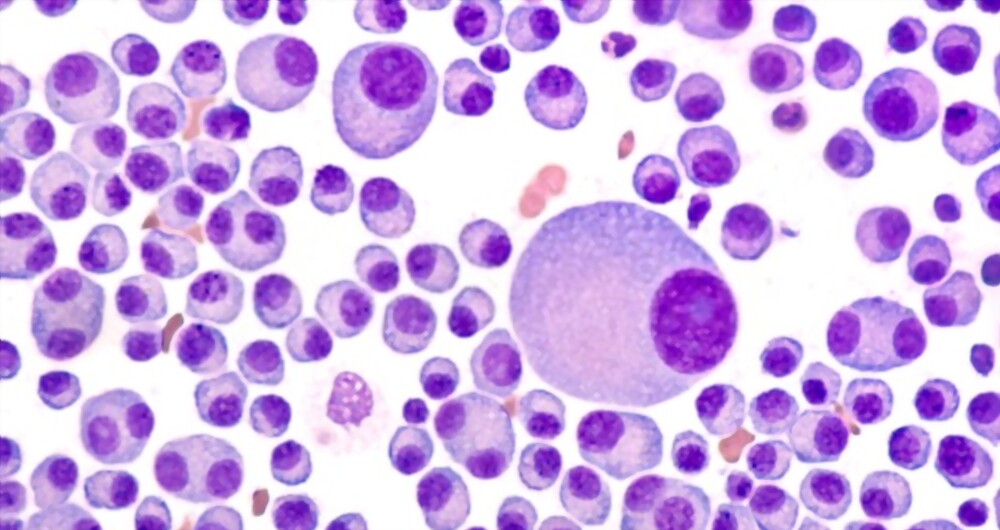
Lymphoma: type of cancer that arising from the infection-fighting cells in immune system called lymphocytes (white blood cell type in the bone marrow)
Lymphocytes function: circulate throughout the body via blood and the lymphatic system; as bacteria and other invaders (pathogenic microbes or foreign substance) are encountered in the lymph fluid, lymphocytes multiply (including B cells, T cells, and natural killer (NK) cells).
How Lymphomas develop? - When the lymphocytes transform from healthy to malignant cells.
How Lymphomas develop? - When the lymphocytes transform from healthy to malignant cells.
Classification for lymphoma - partly classified as B cell lymphomas (the majority/common), T cell lymphomas, or NK cell lymphomas (rare).
Note: Lymphoma is one of the primary cancers to affect children and young adults.
The two main types are:
- Hodgkin lymphoma: only about 10% of patients diagnosed are affected
- non-Hodgkin lymphoma (NHL): vast majority (90%) of lymphoma diagnosed
Hodgkin lymphoma: categorized specifically on microscopy with presence of Reed-Sternberg cells. Reed-Sternberg cells: large, cancerous, B cell-derived cells with a distinct appearance, Hodgkin lymphoma is one of the most treatment-responsive cancer types, even advanced disease are being cured with standard therapies.
Non-Hodgkin lymphoma(NHL): r diverse group of diseases distinguished by the characteristics of the cancer cells associated. Most people with NHL have a B cell type (about 85%), others have a T cell type or a natural killer (NK) cell type of lymphoma. NHL represents a more aggressive cancer ; still certain cases with fast-growing NHL can be completely cured.
Lymphoma Treatment Options (depends on type of lymphoma diagnosed):
- Chemotherapy
- Radiation
- combinations of the two are typically used to treat both types of lymphoma
- Stem cell treatment (in cases initial courses of treatments are ineffective)
- Radiotherapy is used less often (or used typically when the disease is localized to a single site in the body)
- Immunotherapy : class of treatments where patient’ own immune system is used to kill cancer cells. ( currently ten effective FDA-approved immunotherapy options for lymphoma are available)
The hematoncologist will talk to you about using immunotherapy for aiding the treatment regimen in lymphoma of you or your patient. Yes! Surely being promising newer type of cancer treatment; it works with natural immune system to find and kill cancer cells in patients body. For detail and learning about immunotherapy in lymphoma you can consult Dr Gaurav Dixit.
The different kinds of immunotherapy for lymphoma:
- Chemotherapy
- Radiation
- combinations of the two are typically used to treat both types of lymphoma
- Stem cell treatment (in cases initial courses of treatments are ineffective)
- Radiotherapy is used less often (or used typically when the disease is localized to a single site in the body)
Monoclonal Antibodies
- lymphoma cells are tested to see if they have certain markers / proteins called antigens.
- a monoclonal antibody drug aims at the antigens found on lymphoma cells
- Monoclonal antibodies are engineered in lab to lock onto certain antigens that cancer cells and affect mostly cancer cells with little damage to normal cells.
Monoclonal antibodies mechanism of action:
- Restrict the cancer cells from growing by blocking signals sent out by the cancer cells.
- bind to the cancer cells and trigger immune system to kill them.
- Monoclonal antibodies attached to toxins, chemo, or radioactive substances and carry these cell-killing materials to the cancer cells and lock onto the antigen leading to the death of the cancer cells.
- Rituximab (Rituxan) targets the CD20 antigen,
- To target CD20. Other examples are ibritumomab tiuxetan (Zevalin), obinutuzumab (Gazyva), and ofatumumab (Arzerra).
- The monoclonal antibody that targets a different antigen found on lymphoma cells are availaible for instance, alemtuzumab (Campath) incase lymphoma cells have the CD52 antigen.
- lymphoma cells might have the CD30 antigen, in which case brentuximab vedotin (Adcetris), a monoclonal antibody attached to chemo, is part of treatment plan.
Immunomodulating Drugs
- help immune system work better, but how they work exactly is still ongoing research.
- The two drugs are thalidomide (Thalomid) and lenalidomide (Revlimid).
- only get these drugs if one agree to take special precautions to prevent pregnancy because they cause severe birth defects.
Immune Checkpoint Inhibitors:
- Cells proteins referred checkpoints help immune system to differentiate between good and bad cells.
- Lymphoma cells make these checkpoints to trick immune system into not killing them. Immune Checkpoint Inhibitors drugs help keep this from happening.
In multiple myeloma case if no symptoms are experienced (condition also known as smoldering multiple myeloma), one might not need treatment right away. However, regularly monitoring condition for signs and follow up is a necessity, so that the disease is progressing or not can be kept to a vigilant record by your hemato-oncologist.
CAR T-Cell Therapy: very new treatment used for some types of B-cell lymphoma.
- CAR stands for chimeric antigen receptor; engineered in lab
- designed to lock onto antigens found on lymphoma cells
- Each patient has their own unique CAR T cells made just for them.
- some T cells filtered out of patients’ blood are engineered in lab to CARs. Then the lab grows lots of those cells. the CAR T cells after infusion in pataient body travel through blood to find, lock onto, and kill the cancer cells. They also have properties to grow and multiply for months, or maybe even years.
Targeted Antibodies/target drug therapy like:
- Brentuximab vedotin (Adcetris®): targets the CD30 (Hodgkin or non-Hodgkin lymphoma, as a first-line therapy)
- Ibritumomab tiuxetan (Zevalin®): targets the CD20 pathway (non-Hodgkin lymphoma)
- Mogamulizumab (Poteligeo®): targets the CCR4 pathway( two rare types of non-Hodgkin lymphoma—mycosis fungoides and Sézary syndrome—that affect the skin)
- Obinutuzumab (Gazyva®): targets the CD20 pathway (non-Hodgkin lymphoma, including as a first-line therapy)
- Polatuzumab vedotin (Polivy™):targets the CD79b pathway (non-Hodgkin lymphoma)
- Rituximab (Rituxan®): targets the CD20 pathway( CD20-positive non-Hodgkin Lymphoma (NHL), including as a first-line therapy)
- Tafasitamab-cxix (Monjuvi®): targets the CD19 pathway ( diffuse large B-cell lymphoma)
Immunomodulators:
- Nivolumab (Opdivo®): targets the PD-1/PD-L1 pathway (classical Hodgkin lymphoma)
- Pembrolizumab (Keytruda®): targets the PD-1/PD-L1 pathway (classical Hodgkin lymphoma)
- Interferon alfa-2b (Intron A®): targets the IFNAR1/2 pathway (follicular lymphoma)
CAR T-Cell Therapy:
- Axicabtagene ciloleucel (Yescarta®): CD19-targeting CAR T cell immunotherapy (non-Hodgkin lymphoma or follicular lymphoma)
- Brexucabtagene autoleucel (Tecartus™): CD19-targeting CAR T cell immunotherapy (mantle cell lymphoma)
- Lisocabtagene maraleucel (Breyanzi®): CD-19-targeting CAR T cell immunotherapy (large B cell lymphoma)
- Tisagenlecleucel (Kyrmriah®): CD19-targeting CAR T cell immunotherapy (relapsed or refractory large B cell lymphoma)
Request an Appointment with Dr Gaurav Dixit at Action cancer hospital,A-4, Paschim Vihar, New Delhi, Delhi, India 110063.
For consultation please see following contact details:
Dr Gaurav Dixit DM (clinical hematology)
Consultant clinical Hematologist and BMT physician
Action cancer hospital
A-4 Paschim Vihar, New Delhi 110063